#5 Rate Limits and Vaccine Throughputs
My journey down the rabbit hole of understanding throughput values of vaccine delivery at the site level, and the implications for resource allocation, financing, and policy.
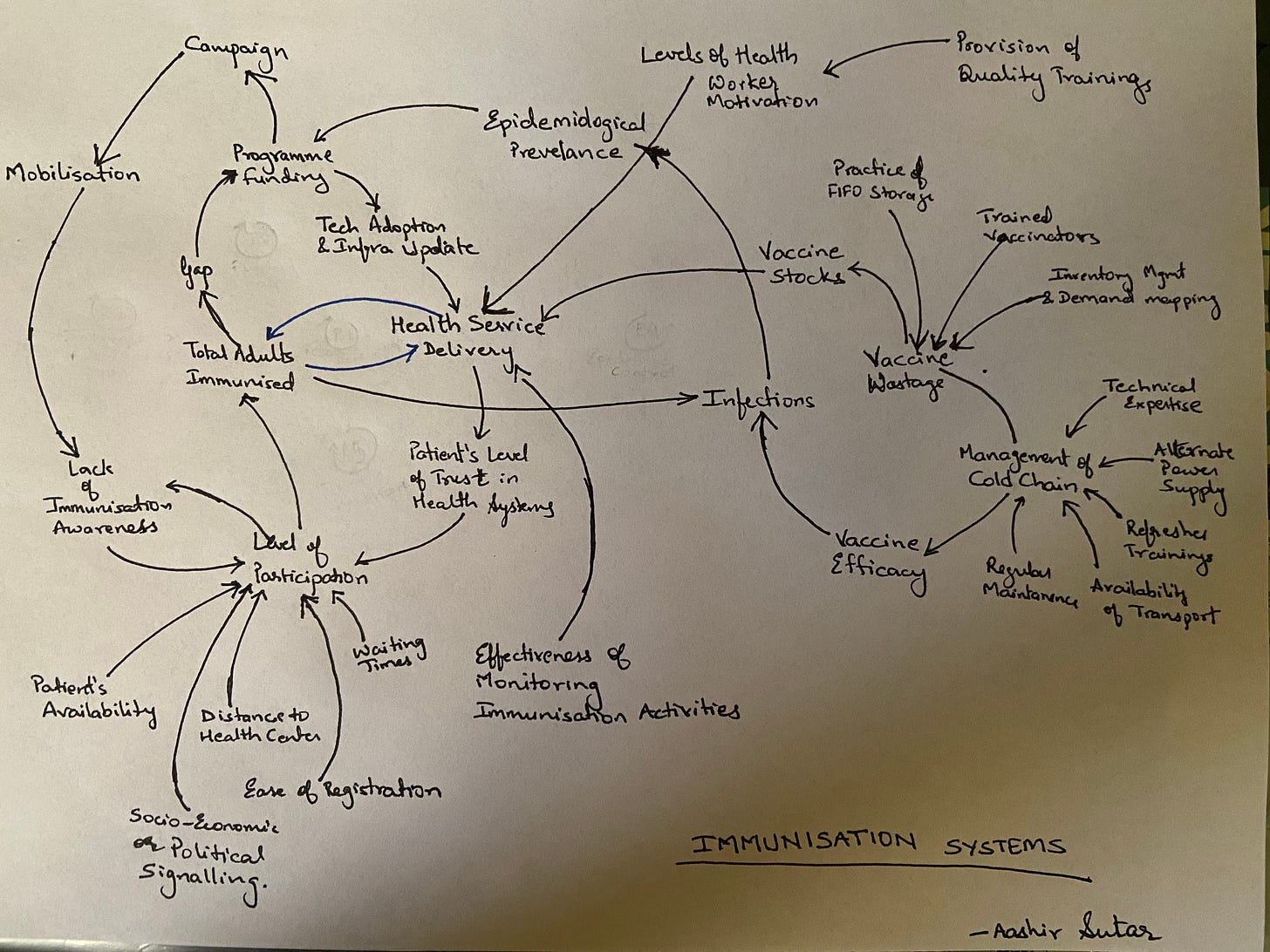
Two weeks ago (5th of June), I did a piece on the systems approach and behavioural economics of vaccine delivery, and the key gaps that plague the system.
#3 Optimum Vaccine Delivery for COVID 19 - A Systems Approach
A systems thinking and behavioural economics perspective towards understanding the underlying vaccine delivery systems for COVID-19, and the key gaps that plague us even today.
As a follow-up, I write this post that digs deeper into the core vaccine delivery operationalisation, the impact of rate limits on the field implementation, and an attempt to understand how resource allocation (especially financial resources) has cascading changes in the vaccination rates. For this, I analyse the district level vaccine data since the beginning of the year 2021. For this post, however, I focus on the period starting 1st June to 17th June (the day I write this post).
Meta:
I was fascinated with the vaccine delivery dataset, and the chaos ensuing around vaccine delivery over the past couple of months. Even after delayed purchases and the recent move of going back to the centralised procurement, I oft wondered why are we doing what we are doing. So this is an attempt to deconstruct the core system from first principles thinking, and understanding what I call “rate limits” of a system (covered in the last post).
Every entity in an existing system has an inherent capacity to provide or receive attributes. This is called the Rate Limit.
Why is it important:
Throughput Values indicate the rate of change, which directly impacts procurement as well as delivery, and a lot of decisions on resource allocation in between.
Optimise Throughput per session: Ensure each session has at least one vaccine officer (VO), who is able to achieve 45 doses per day. Currently, this is a huge gap.
Optimise VO per site: It is important to balance the number of inoculators at the site level vs the number of doses to be administered. While optimising every vaccine session, it is also important to optimise the VO per site, so as to conduct more sessions and deliver more doses.
Increase sessions per site: A natural follow-up to point 3 is to increase the number of sessions per site. This is a critical resource allocation decision that has an impact on the marginal and overhead costs, and has a direct impact on the vaccine inventory.
Increase number of sites: Tap into the unused public health infrastructure to increase the number of sites engaged in vaccine delivery. This will have a cascading impact on the number of people getting inoculated, anywhere between say 3000 to 50,000 per day. This is also accompanied by a large fixed cost and systems setup. However, ensuring points 1 through to 4 will help optimise the cost and get the best performance.
District Level Vaccine Allotment: I did mention in my previous post that the allotment of vaccines per district has other systemic factors impacting the outcome, but none more than reducing capacity wastage and optimised resource allocation to increase the demand generation, which eventually will help increase the vaccine allotment at the district level.
Annex -1: Governing Dynamics of Vaccine Delivery
We take vaccine doses entering the site as the point of entry, at say time T=0. The site allocates its resources based on the number of vaccine doses in its inventory. It allocates nurses and the support staff, along with a limited set of doses to administer.
The rate limits on this system are pretty straightforward. A vaccine officer (VO) or an inoculator can only administer the doses at the maximum rate of 45-50 doses per day. We call this value “Vaccine Throughput per Inoculator”, which means the rate of doses delivered to people in a specific time period (one working day of 8 hours) by a single inoculator.
An excerpt from an EY report “Protecting India: Public Private Partnership for vaccinating against COVID-19” published in December 2020, in collaboration with FICCI.
• Maximum potential of 10-15 doses per hour basis interviews with public health experts and medical administrators of private hospital chains
• 4-5 minutes per inoculation (basis expert interviews) includes pre-inoculation time (record history/ skin-prick allergies (if any)/ vital signs, prepare for inoculation), inoculation time and post-inoculation time (dispose syringe/ needle, handover inoculation certificate and instructions w.r.t next dose and steps in case of AEFI)
• Actual throughput at the site expected to be lower than the max. potential owing to varying inoculator skill-level and the highly decentralized network of centers to cater to the country's geographical spread
• Two doses/ individual within a gap of 3-4 weeks considered as is the prescription in most vaccines at advanced stages of clinical trials
Based on the number of inoculators, the site managers allocate the part of the inventory of doses to administer. Once the doses are administered, the data is collected and fed into the central system that then shows the levels remaining inventory of doses, and also sends a copy of the vaccine delivery to the district administration.
Depending on the type of site, the sites then place an order for vaccinations.
Private Hospitals: In the case of a private site, they place the order directly through the centralised portal. These private sites have to be registered with Pradhan Mantri Jan Arogya Yojana (PM-JAY), the Ayushman Bharat scheme.
Public Health Sites: They report to the district health officer and the other officials of the health department and the district collectorate who then place the order for vaccinations.
This is the entire cycle of events that move from T=0 to T=1, being the next day.
Annex -2: Vaccine Throughput Analysis at District Level
The dataset reports on the following parameters:
Total Individuals Vaccinated (Earlier was Total Individuals Registered)
Total Sessions Conducted
Total Sites
First Dose Administered
Second Dose Administered
Male(Individuals Vaccinated)
Female(Individuals Vaccinated)
Transgender(Individuals Vaccinated)
Total Covaxin Administered
Total CoviShield Administered
The initial problem with this dataset was the fact that the entire data variable of total individuals vaccinated did not account for people taking second doses. Hence, to calculate the throughput, I added data variables 4 and 5, to get a composite number that showed the total doses administered in the district.
In my journey down the rabbit hole to understand vaccine throughput, the following points emerged
The ceiling of maximum doses administered, and deviation from Median
For the period of 1st June to 17th June, I calculated the maximum ceiling of the total number of doses administered in the city, followed by taking the median value of the total number of doses administered in the city for the same time duration. The results were fascinating.
Some of the major cities in India are performing below their maximum capacity that already exists and have been achieved in the same month of June 2021 itsef. To the tune of at least 1 lakh doses per day.
And this is not counting the deficit in the actual required capacity of vaccination at the district level.
Number of Doses administered per Session
This is the doses throughput value per session. Ideally, the benchmark of this value should be 45 doses per session. In the snapshot below, we see multiple districts of Jharkhand with below 20 doses as the median value of doses administered per vaccination officer.
Number of Sessions per Site
A straightforward metric that allows us to understand the distribution of sessions w.r.t the number of sites. The actionable intelligence this metric gives is the estimate of the peak capacity to absorb the fixed cost (of the vaccination site). The snapshot below shows the trends in the state of Tamil Nadu, that have a higher median of sessions per site than most states. One of the reasons this is the case is because a major part of the vaccine delivery process is undertaken by the public health institutions themselves, rather than the private players. An interesting case of Madurai where the median throughput metric of sessions per site actually is higher than the maximum threshold.
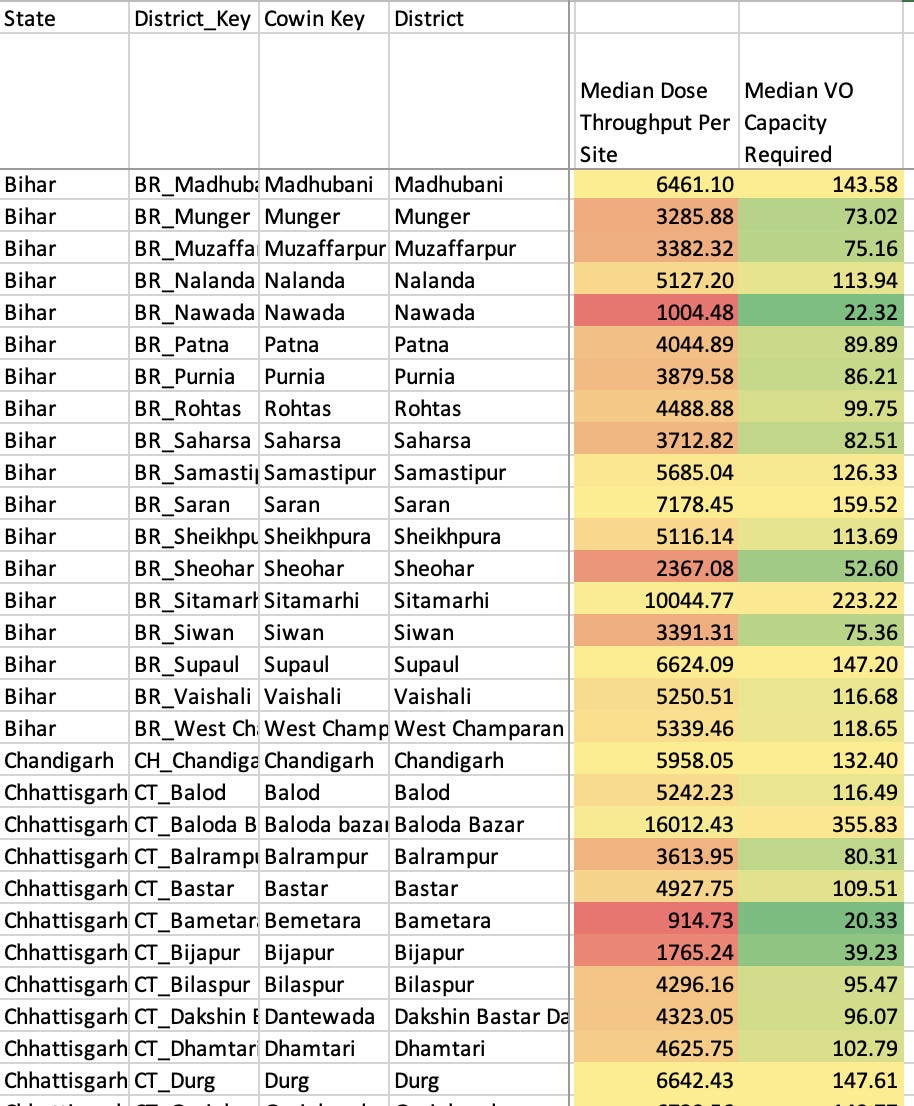
Number of Doses administered per Site
This provides an estimate of the performance of the vaccine delivery w.r.t the fixed cost of the site. This is critical from the resource allocation perspective, where we would like to lower the cost structures at the site level (especially the marginal costs of per dose delivery). In the snapshot below, we see the performance of some of the major districts in Bihar and Chhatisgarh with low values of this throughput metric than other districts in India. This shows we need investment in building the capacities of the sites in these districts to be able to increase their throughput per day.
The metric of median VO capacity indicates the median value of the number of vaccination officers required in a particular district based on the present availability of vaccines. This also estimates the variable cost incurred by the vaccine sites. This also provides us with estimates of the impact of the fixed cost investment w.r.t the number of doses administered.
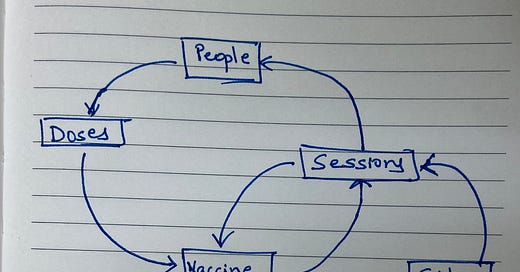
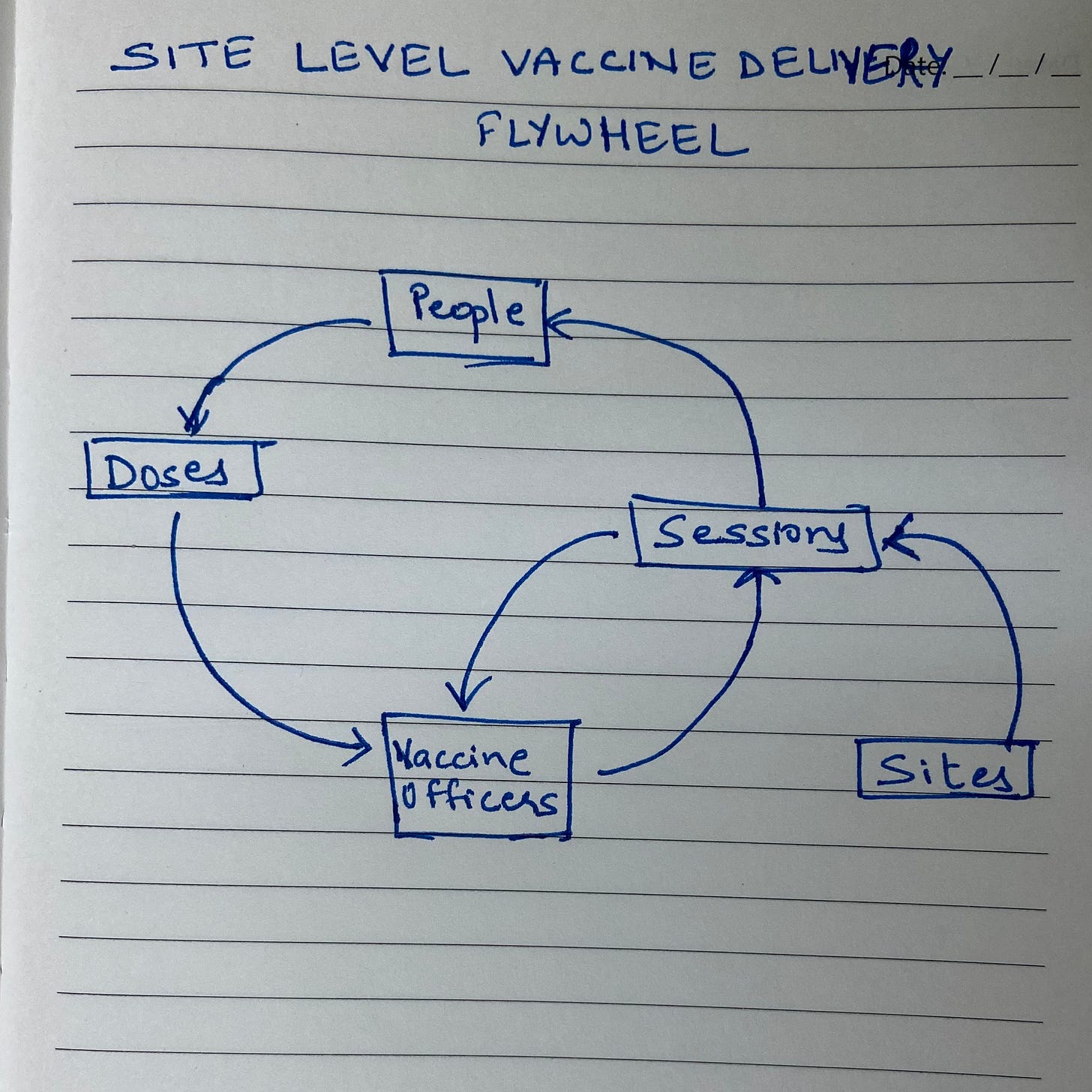
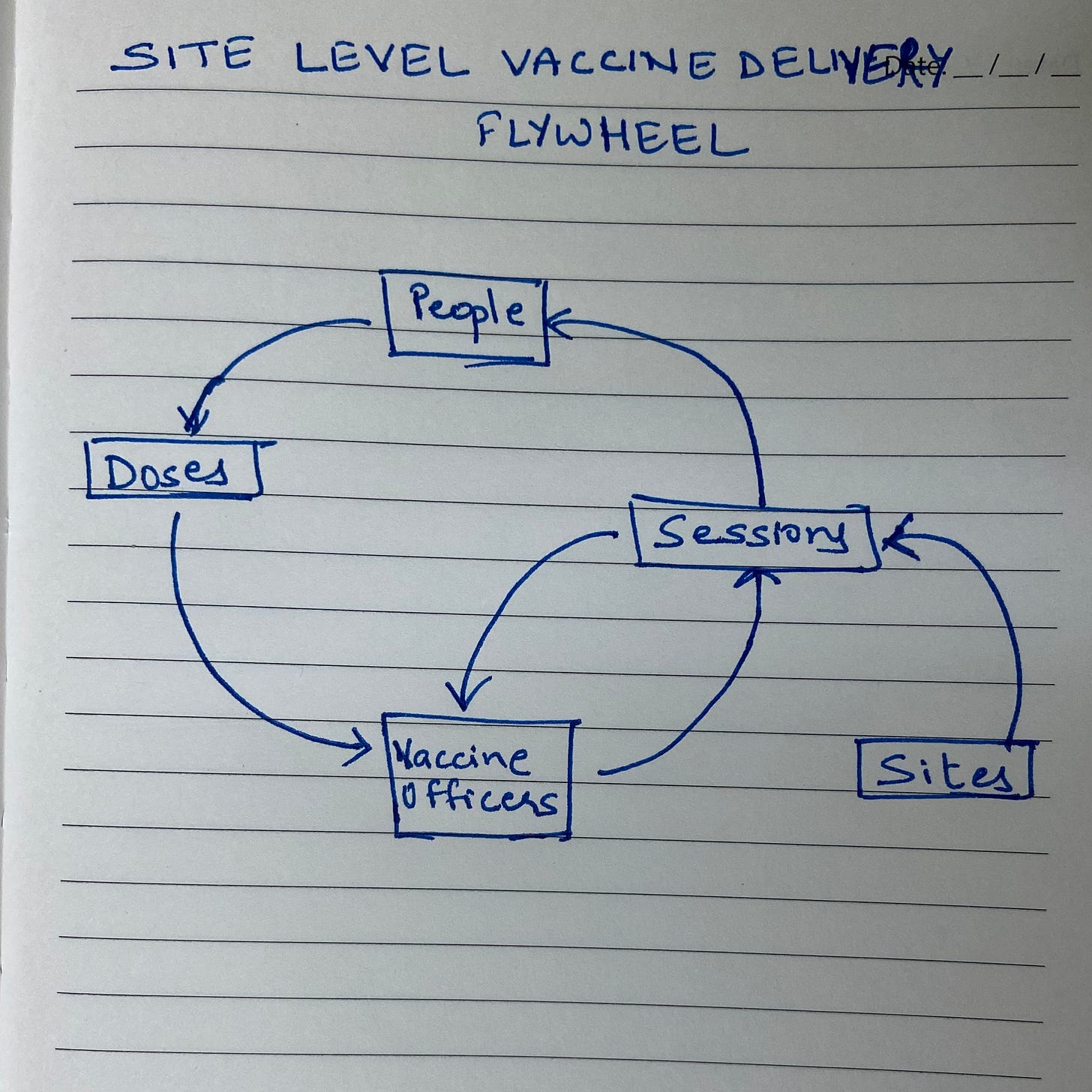
Annex-3: Last-mile Vaccine Delivery Flywheel
In my previous post “#3 Optimum Vaccine Delivery for COVID 19 - A Systems Approach”, I had used the following systems diagram to provide a high-level view of the interconnected system of vaccine delivery.
However, in this post, we delve deep into just the last-mile delivery phase to deconstruct the core system. The illustration below is the systems view of the vaccine delivery process
The flywheel of the vaccine delivery components consists of the following critical components:
Sessions and Sites: Basic unit of vaccine delivery. Each “session” happens at a “site”, which send-in data and report to the district administration. These sites can be public health infrastructures like Primary Health Centers, Sub Centers, District Hospitals, etc; or these sites can be private hospitals with the necessary permission from the district administration. These “Sites” are important to understand, as they are the only people that help with the demand generation of the COVID-19 vaccine, which then directly affects the procurement of the vaccines in a particular district. There are various types of sites, which can either be:
Fixed Session Site: These sites include health facilities – both government and private – where either a medical officer or a doctor is available is defined as a fixed session site
Outreach Session Site: Locations other than health facilities such as schools, community halls, come under this list
Special Mobile Team: For remote, hard-to-reach areas, migratory populations areas and international borders areas, district administrations will plan the vaccination drive via the special mobile team
People: These are the people that desire to get vaccinated, and are registered on the CoWIN portal (or are walk-ins).
Doses: These are the doses procured and delivered to the “sites”, which are administered to the people through “sessions”.
Inoculators: Any individual who is authorised to administer a vaccination, which can be a doctor (MBBS/BDS), staff nurse, pharmacist, auxiliary nurse midwife (ANM), or a lady health visitor (LHV).
COVID-19 Vaccines Operational Guidelines: The vaccination team will consist of five members as follows:
Vaccinator Officer–Doctors (MBBS/BDS), staff nurse, pharmacist, auxiliary nurse midwife (ANM), lady health visitor (LHV); anyone authorized to administer an injection may be considered as a potential vaccinator;
Vaccination Officer 1: At least one person (Police, home guard, civil defense, national cadet corps (NCC), national service scheme (NSS), endr yuva kendra sangathan (NYKS) who will check the registration status of a beneficiary at the entry point and ensure the regulated entry to the vaccination session;
Vaccination Officer 2: Is the verifier who will authenticate/verify the identification documents;
Vaccination Officer 3 & 4 are the two-support staff who will be responsible for crowd management and ensure 30 minutes of waiting time by beneficiary post-vaccination. Support staff will provide information, education and communication (IEC) messages and support to vaccinator as well as the vaccination team.